Diabetes mellitus is a group of metabolic diseases characterized by high levels of glucose ("sugar") in the blood.
Why we need glucose
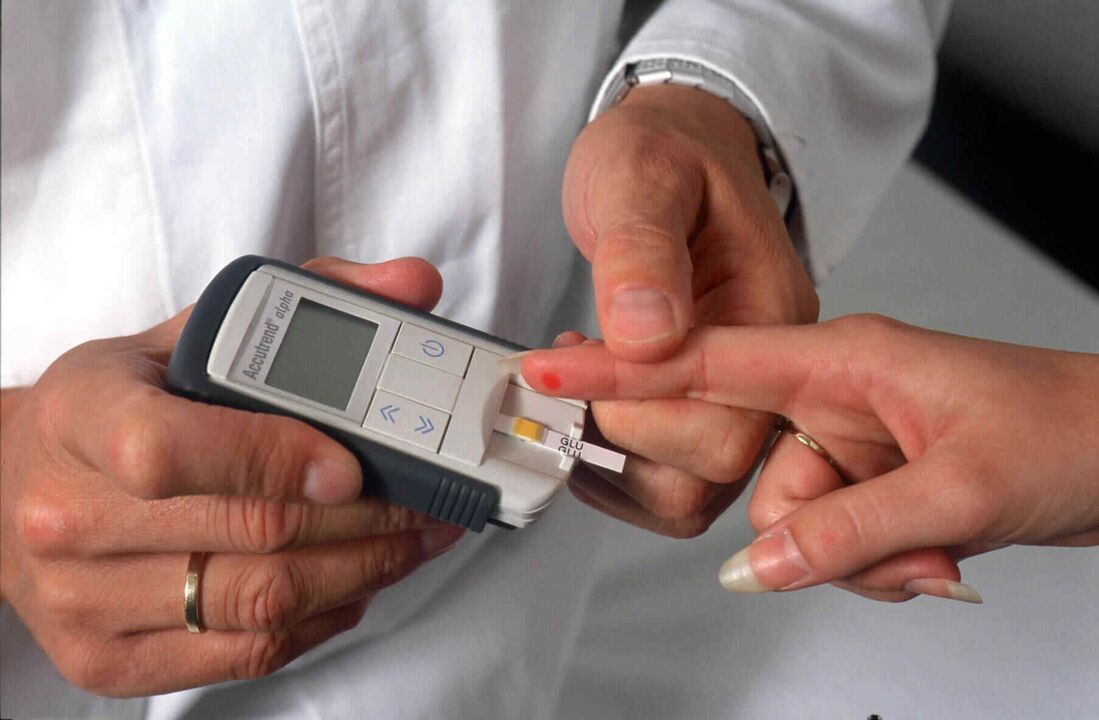
The norm of glucose (sugar) in whole capillary blood is 3. 3-5. 5 mmol/l in the morning on an empty stomach (i. e. after 7-14 hours of fasting) and up to 7. 8 mmol/l after eating (i. e. 1. 5). -2 hours after the last meal).
Normally, in the human body, the cell uses glucose as a source of energy (in other words, the body's cells "feed" on glucose from the blood). The more the cell works, the more energy (glucose) it needs.
Glucose (the term "blood sugar" is more often used, but this is not entirely accurate) is constantly circulating in the human blood. There are 2 ways for glucose to enter the human body: - the first is through food containing carbohydrates, - the second is through the production of glucose in the liver (this is the reason that in diabetes mellitus, even if the patient has not eaten anything, the level of glucose in the blood canbe increased).
However, to be used as energy, glucose from the blood must go to the muscles (to do work), adipose tissue, or the liver (the body's store of glucose). This happens under the influence of the hormone insulin, which is produced by the beta cells of the pancreas. As soon as blood glucose levels rise after a meal, the pancreas immediately releases insulin into the blood, which in turn binds to insulin receptors on muscle, fat or liver cells. Insulin, like a key, "opens" the cells to allow glucose to enter them, resulting in the normalization of blood glucose (sugar) levels. Between meals and at night, if necessary, glucose enters the blood from the liver depot, so at night insulin controls the liver so that it does not release too much glucose into the blood.
If there is a violation at any stage of this process, diabetes mellitus occurs.
Types of diabetes
Diabetes mellitus type 1 (previously used name: insulin-dependent diabetes mellitus) develops mainly at a young age (usually before the age of 30, although type 1 diabetes mellitus can also develop at a later age).
Type 1 diabetes mellitus is caused by the cessation of insulin production in the pancreas due to the death of β-cells (responsible for insulin production in the pancreas). The development of type 1 diabetes mellitus occurs against the background of a special genetic predisposition (that is, a person is born with it), which, when exposed to some external factors (for example, viruses), leads to a change in the state of the body's immune system. The body of a patient with type 1 diabetes begins to perceive his pancreatic β-cells as foreign and protects against them by producing antibodies (similar to what happens when protecting against infection), which leads to the death of pancreatic β-cells, which means severe insufficiencyinsulin.
Diabetes mellitus 1 type develops when at least 90% of pancreatic β cells die. Let's recall the mechanism of action of insulin, its function as a "key" that opens cells for sugar. In type 1 diabetes, this key has disappeared from the blood (see picture).
Insulin deficiency in type 1 diabetes mellitus The onset of type 1 diabetes mellitus is acute, always accompanied by severe symptoms of hyperglycemia (high blood sugar): - weight loss (patient loses weight involuntarily), - constant feeling of hunger, - thirst, dry mouth (patientdrinks a lot of fluids, including at night), - frequent urination (in regular or large portions, including at night), - weakness.
If you do not consult a doctor in time and do not start treatment of type 1 diabetes with insulin, the condition worsens, and very often a diabetic coma develops.
Diabetes mellitus type 2 (previously called insulin-dependent diabetes mellitus) is much more common than type 1 diabetes mellitus. The incidence of type 2 diabetes mellitus is typical for older people: it is detected, as a rule, after 40 years of age, although recently, according to WHO experts, the average age of patients with type 2 diabetes mellitus is getting younger.
About 80% of people with type 2 diabetes are overweight. Also, type 2 diabetes is characterized by heredity - high prevalence among close relatives.
In type 2 diabetes, the pancreas continues to produce insulin, often in larger amounts than usual. Although there are also cases of diabetes mellitus type 2 with reduced insulin secretion.
The main defect in type 2 diabetes is that the cells do not "feel" insulin well, that is, they do not open well in response to the interaction with it, so the blood sugar cannot fully penetrate (see picture). The level remains elevated. This conditionreduced sensitivity to insulin is called insulin resistance.
Low sensitivity to insulin in type 2 diabetes mellitus You can vividly imagine that the "keys" (scientifically speaking - insulin receptors) on the doors of the cells are deformed, and there is no perfect match with the keys - insulin molecules. More effort is required (more keys, i. e. more insulin) to overcome the insulin receptor defect. The pancreas cannot deliver a sufficient amount of insulin to the blood to overcome insulin resistance and completely normalize the blood sugar level, because in diabetesmellitus type 2, the capabilities of β cells are still limited.
As a result, in type 2 diabetes, a paradoxical situation arises when there is a lot of insulin and sugar in the blood at the same time.
Diabetes mellitus type 2, unlike diabetes mellitus type 1, begins gradually, often completely unnoticed by the patient. So, a person can be sick for quite a long time, but not know about it. Elevated levels of sugar (glucose) in the blood may be detected accidentally during a check-up for another reason.
At the same time, there are cases with clear manifestations of hyperglycemia:
- weakness, fatigue, thirst, dry mouth (the patient drinks a lot of liquids, including at night),
- frequent urination (regular or in large quantities, including at night),
- itching of the skin (especially in the perineal area),
- slow wound healing, - frequent infections, - blurred vision.
Diabetic coma develops much less often, usually if diabetes mellitus type 2 is accompanied by some other very serious disease: pneumonia, severe injuries, purulent processes, heart attack, etc.
Treatment of diabetes
Treatment for diabetes varies depending on the type of diabetes.
In diabetes mellitus type 1, which occurs as a result of absolute insufficiency of insulin secretion by the pancreas, constant self-monitoring and treatment with insulin is required to preserve life. It should be emphasized that exogenous insulin treatment is the only treatment option in this situation. The selection of doses and regimens for the treatment of diabetes mellitus with insulin is carried out individually, taking into account age, sex, physical activity and individual sensitivity to insulin.
For type 1 diabetes mellitus sometimes, at the very beginning of the disease, after the normalization of blood glucose during the treatment of diabetes mellitus with insulin, the need for it suddenly begins to decrease until it is completely canceled. But this is not recovery. This phenomenon is called the "honeymoon" of diabetes, or scientifically remission. This is explained by the fact that after blood sugar is normalized with the help of insulin, β cells that have not yet died can work for a while. After that, everyone dies, and the person needs lifelong insulin treatment for diabetes mellitus. Anyone who gets type 1 diabetes for the first time, the doctor should warn about the possible occurrence of such a situation and what to do in that case.
Diabetes mellitus can be treated with insulin using insulin syringes, pens or an insulin pump.
Insulin pump therapy is an alternative treatment for diabetes in people who frequently use a syringe or pen to inject insulin and regularly measure their blood sugar levels. Instead of treating diabetes with injections, insulin pump therapy is used. The pump is worn on the body or on clothing, for example, on the belt. Currently, about 250, 000 people around the world use insulin pumps.
The main goal of type 2 diabetes treatment is to improve the sensitivity of cells to insulin. The causes of poor insulin sensitivity are not yet fully understood. However, it has long been known that the most powerful factor in the formation of insulin resistance is excess weight, i. e. excessive accumulation of fat in the body. Numerous scientific studies and long-term observations of patients show that weight loss during the treatment of type 2 diabetes can achieve a significant improvement in blood sugar levels in most patients.
In type 2 diabetes, normalization of body weight can lead to complete normalization of blood sugar for a long time, although this cannot be called a complete recovery.
If diet and exercise aimed at losing weight do not give sufficient effect in the treatment of type 2 diabetes, you must resort to medication. They are available in tablets. Some of them act on the pancreas, increasing the production of insulin, while others improve its action (reduce insulin resistance). Therefore, the drugs used to treat type 2 diabetes mellitus do not lower blood sugar, insulin does, so in order to achieve the effect of tablets in the treatment of diabetes mellitus, a preserved reserve of β-cells of the pancreas is necessary. This makes it clear why it is pointless to use tablets in the treatment of type 1 diabetes, because most of the β cells have already died.
Insulin is often used to treat type 2 diabetes. Insulin therapy for type 2 diabetes mellitus may be prescribed as a temporary measure, for example, during surgery, severe acute illnesses, or as permanent therapy. Therefore, it is not currently recommended to call type 2 diabetes mellitus insulin-dependent. The type of diabetes treatment does not determine the type of diabetes.
Diet plays the most important role in the treatment of diabetes.
Diet for diabetes
Despite common goals in the treatment of different types of diabetes (elimination of symptoms of high blood sugar, minimizing the risk of hypoglycemia, prevention of complications), dietary patterns for type 1 and type 2 diabetes mellitus differ significantly. There is no single diet plan for diabetes mellitus.
In diabetes mellitus type 1, the appearance of which is associated with the death of beta cells of the pancreas and lack of insulin, the main method of treatment is insulin replacement therapy, and dietary restrictions, according to modern views, are of an auxiliary nature and should be given only to the extent that insulintherapy differs from insulin production in a healthy person.
The basic principles of prescribing a diet for type 1 diabetes mellitus have undergone critical revision in recent years.
One of the principles of the traditional diet for diabetes is the recommendation to consume a strictly defined, identical amount of calories every day. Each patient is prescribed a daily calorie requirement based on an "ideal weight". This makes no sense and is impossible for the following reasons:
- In healthy individuals of normal weight, the balance between energy intake and expenditure varies widely from day to day. Energy consumption in healthy people is variable because their physical activity is variable. Consequently, if you prescribe a given diet for a patient with type 1 diabetes with the daily consumption of a fixed, identical amount of calories, then you would have to recommend an equally given, strict physical activity plan to maintain a normal weight. for every day, which is absolutely unrealistic.
- In patients with type 1 diabetes mellitus with normal weight and a properly selected insulin treatment regimen for diabetes mellitus, appetite regulation does not differ from that of healthy individuals. The fact that they sometimes have to force themselves to eat in order to prevent hypoglycemia, even in the absence of appetite, is most often a consequence of insufficient insulin therapy.
Improved treatment regimens for diabetes mellitus using insulin and self-monitoring of metabolism based on blood sugar levels give the patient the ability to regulate food intake only depending on feelings of hunger and satiety, like healthy people. Thus, the diet of a patient with type 1 diabetes mellitus corresponds to a complete healthy diet (balanced in terms of calories and content of essential nutrients). The only difference is that the injected insulin does not "know" when and how much you eat. Therefore, you must ensure that the action of insulin corresponds to your diet. Therefore, you need to know which foods increase blood sugar.
The main method of treating type 2 diabetes is to normalize body weight through a low-calorie diet and increased physical activity. Diet for type 2 diabetes is very important, it is one of the important components that allows you to achieve success.
All food products consist of three components: proteins, fats and carbohydrates. All contain calories, but not all raise blood sugar.
Only carbohydrates have a pronounced effect on increasing blood sugar. What foods contain carbohydrates? It's easy to remember: most products are plant-based, and animal-based - only liquid dairy products. It is important to know if your blood sugar rises after certain foods, and if so, by how much. There are types of carbohydrate foods after which blood sugar either does not rise at all or rises only slightly.
All carbohydrates can be roughly divided into two groups: those containing rapidly absorbed ("fast") carbohydrates and slowly absorbed ("slow") carbohydrates. Products with "fast" carbohydrates contain refined sugars and include preserves and jams, candies, sweets, fruits and fruit juices. "Fast" carbohydrates cause a sudden rise in blood sugar (depending on the amount of food eaten) because they are quickly absorbed into the blood, soit is better to exclude them from the diet for diabetes. "Slow" carbohydrates are much more useful for patients with diabetes, because they take much longer to be absorbed. In addition, the absorption of sugar is slowed down by the fibers found in food, so the diet during the treatment of diabetes should be enriched with foods rich in fiber.
Here are some simple rules to follow when treating diabetes: food should be taken in small portions and often (4-6 times a day); adhere to a fixed diet - try not to skip meals; do not overeat - eat as much as recommended by your doctor; use wholemeal or bran bread; vegetables (except potatoes and legumes) should be eaten daily; Avoid eating "fast" carbohydrates.
Exercise in diabetes Physical exercise in the treatment of diabetes is very important: it increases the sensitivity of body tissues to insulin and thus helps to reduce blood sugar levels.
Housework, walking and running can be considered physical activity. Preference should be given to regular and dosed physical activity: sudden and intense exercise can cause problems with maintaining normal sugar levels.
If you are an athlete, you have no contraindications for playing sports, provided that your blood sugar level is well controlled and all necessary measures are taken to prevent its significant decrease.
Prevention of diabetes complications Patients with diabetes have an increased risk of developing complications on the heart and blood vessels (especially in the legs and kidneys). Regular physical activity, sometimes just walking, is enough to prevent circulation problems in the feet.
If you have diabetes, an untreated wound or scratch on your foot can develop into a serious problem. Even minor cuts or scrapes on the feet take longer to heal than in non-diabetic patients and require more attention. The key to preventing these problems is wearing well-fitting shoes and checking your feet often. Use a mirror if you find it difficult to examine all parts of your feet and remember that foot injuries are often painless at first and can go unnoticed for a long time if you are not careful enough.
Patients with diabetes have an increased risk of kidney dysfunction and heart disease several years after diagnosis. There is good evidence that good blood sugar control reduces this risk. Also, in order to prevent complications of diabetes mellitus, preventive treatment is required 2 times a year.
Blood pressure control is also important. Check your blood pressure regularly. If it is elevated, your doctor will prescribe treatment.

























